This story was originally published by Mountain State Spotlight. Get stories like this delivered to your email inbox once a week; sign up for the free newsletter at https://mountainstatespotlight.org/newsletter
By Allen Siegler, Mountain State Spotlight
With West Virginia’s multiple recent HIV outbreaks and overdose crisis that has impacted residents for decades, many health experts believe the state is in dire need of needle exchange programs. But for the last few years, its politicians have questioned whether the programs are effective and whether they’ve made communities more dangerous.
Often, elected officials share anecdotes about rising crime and finding drug-related litter in community spaces to support decisions that make it harder to exchange used needles for clean ones. But decades of research have found that needle exchanges are an effective tool to support communities’ health and, if anything, decrease litter and crime.
Here’s what needle exchange programs are, why public health practitioners use them, how they’ve affected communities and how they’re being used throughout West Virginia.
What are needle exchanges? Why do they exist?
Needle exchanges, also known as syringe service programs, have been around since at least the 1980s, a few years after scientists first determined HIV could be transmitted by sharing needles. They were initially set up in cities like San Fancisco and Boston — swapping used syringes and needles for clean ones to protect people who inject drugs from the virus.
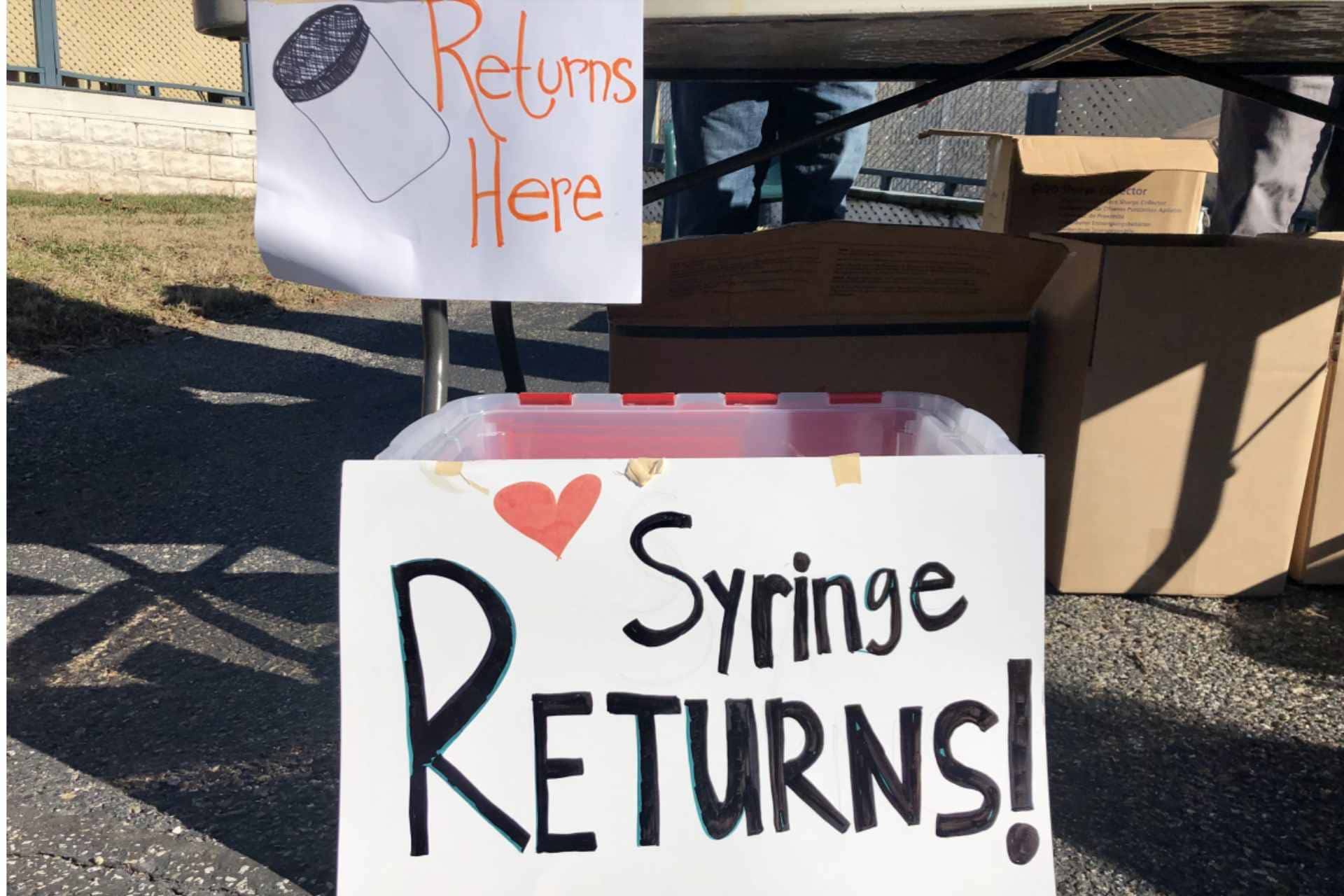
Now, they’ve evolved to be one component of broader harm reduction programs that often offer a variety of health services like HIV testing, hepatitis vaccinations, fentanyl test strips and substance use disorder treatment referrals. All of the services are aimed at keeping people from overdosing, protecting people from diseases and connecting those who might not be comfortable in a hospital with medical providers.
As HIV has spread to more rural areas, needle exchanges have followed. In 2014, when a large rural HIV outbreak emerged in Scott County, Indiana, it was illegal to operate a needle exchange in the state. A few months later, then-Gov. Mike Pence and the state government took steps to legalize the operations, allowing Scott County’s health department to create a program.
Are needle exchange programs effective? What happens if they go away?
There are many ways syringe service programs can be run. But as a whole, public health researchers have found them to be effective tools for keeping people who use drugs safe and healthy. Programs not only prevent the spread of blood-borne diseases like HIV and hepatitis C but also can lead people who use drugs to start substance use disorder treatment.
The Scott County, Indiana program showed that syringe services can have a lot of success in rural settings as well. Shortly after it opened and HIV treatment options became more available, HIV cases declined dramatically. Epidemiologists who’ve studied the outbreak have also found evidence that had the syringe service program been opened earlier, there may have never been a crisis in the first place.
Scientists have also researched what needle exchanges don’t do. As a whole, syringe services do not lead to increased crime, drug use or litter in communities where they operate.
Kanawha County has recently experienced the effects of what happens when a needle exchange goes away. In the years since the state Department of Health and Human Services suspended the local health department’s syringe services in 2018, the county’s HIV cases multiplied, leading to an outbreak.
In a report on the closure, the Centers for Disease Control and Prevention said making it easier for Kanawha residents to access clean needles would be crucial for reducing the spread of the virus.
How do needle exchanges work in West Virginia?
At the end of 2022, there were nine authorized syringe service programs in West Virginia, according to state data. Most of them are in permanent locations but a few, like the Fayette County Health Department, have begun running mobile operations to reach more people. The programs cannot use federal dollars to buy syringes or needles and seek out private funding for those supplies.
There used to be more programs in West Virginia; reports show that in 2019, there were twice as many operating throughout the state. But a number of programs shut down after state legislators passed Senate Bill 334, a law that added many restrictions to how West Virginia needle exchanges can be run and who can access them.
What is and isn’t allowed in West Virginia?
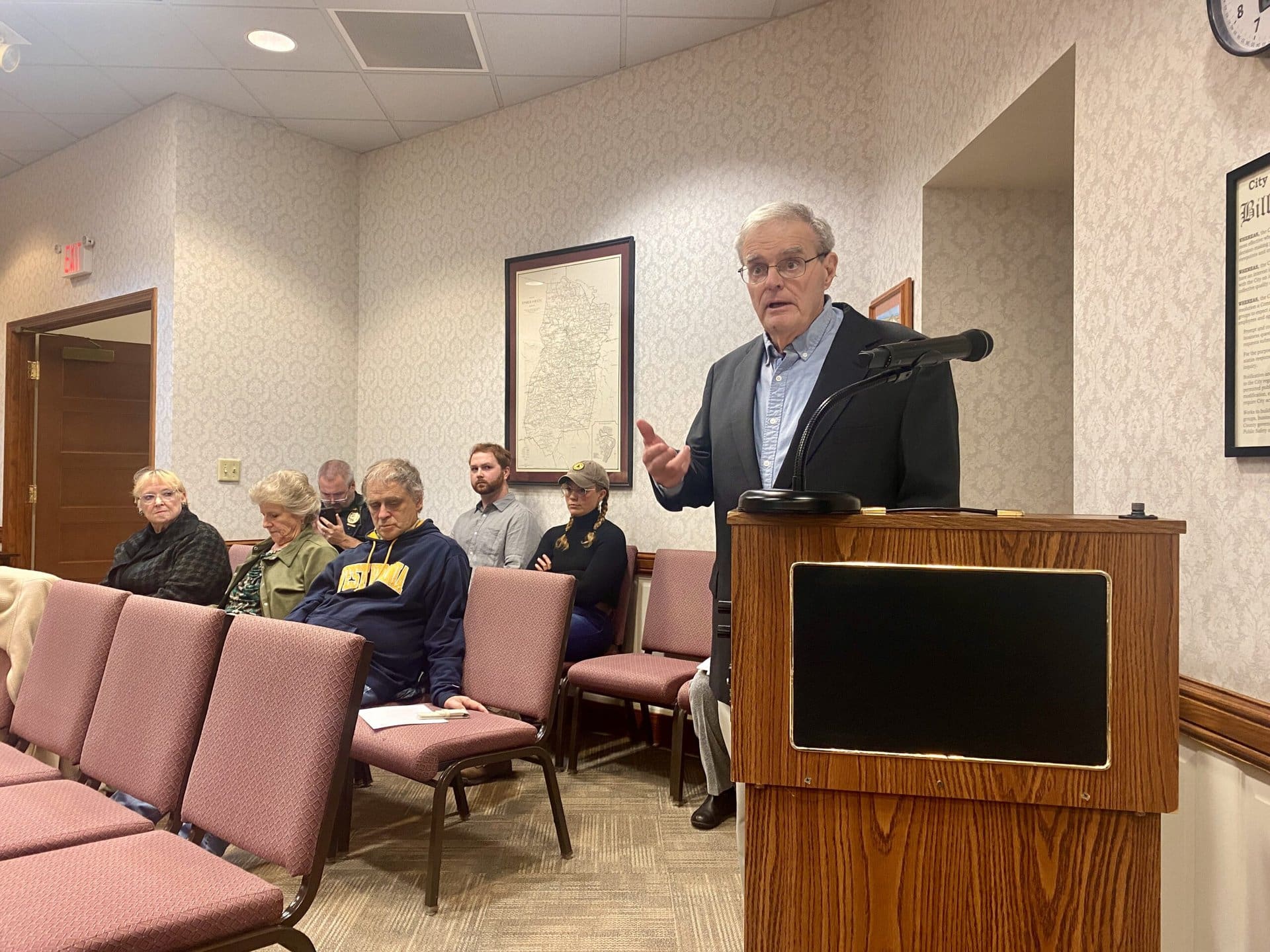
SB 334 puts limits on how syringe service programs can be run. All programs, both ones that existed prior to the law’s passage in 2021 and ones that were created afterward, must receive approval from both the city council and county commission where they operate. Either government can revoke a program’s license or deny applications for new ones.
The bill also requires each syringe service program to offer or refer participants to 10 different types of health services that range from education about infectious disease transmission to birth control.
Anyone who would like to use a syringe service program must be at least 18 and prove West Virginia residency with a state-issued ID card or utility bill. SB 334 also requires the program’s administrators to try to take back as many needles as they give out.
West Virginia’s law runs contrary to the recommendations of the U.S. Office of National Drug Control Policy. In its model law for how states should govern syringe service programs, it writes that programs should be able to distribute “quantities sufficient to ensure that hypodermic needles, syringes, and other supplies are not shared or reused.” The document cites West Virginia’s SB 334 as an example of a law that creates barriers to running successful harm reduction programs.